Diagnostic tests
Bone mineral density: testing for osteoporosis
- Angela Sheu, Terry Diamond
- First published 1 April 2016
- Aust Prescr 2016;39:35-9
- 5 January 2022
- DOI: 10.18773/austprescr.2016.020
Primary osteoporosis is related to bone loss from ageing. Secondary osteoporosis results from specific conditions that may be reversible.
A thoracolumbar X-ray is useful in identifying vertebral fractures, and dual energy X-ray absorptiometry is the preferred method of calculating bone mineral density. The density of the total hip is the best predictor for a hip fracture, while the lumbar spine is the best site for monitoring the effect of treatment.
The T-score is a comparison of the patient’s bone density with healthy, young individuals of the same sex. A negative T-score of –2.5 or less at the femoral neck defines osteoporosis.
The Z-score is a comparison with the bone density of people of the same age and sex as the patient. A negative Z-score of –2.5 or less should raise suspicion of a secondary cause of osteoporosis.
Clinical risk calculators can be used to predict the 10-year probability of a hip or major osteoporotic fracture. A probability of more than 5% for the hip or more than 20% for any fracture is abnormal and treatment may be warranted.
Osteoporosis is a common systemic skeletal disorder leading to decreased bone strength and increased susceptibility to osteofragility fracture. It is a significant health issue that affects up to one million Australians.1
Primary osteoporosis refers to bone loss that occurs due to the normal ageing process, while secondary osteoporosis results from specific clinical disorders that are potentially reversible. Correctly treating an underlying cause may ameliorate fracture risk and avoids unnecessary treatment with antiresorptive drugs.
The diagnosis of osteoporosis is based on the presence of a fracture after minimal trauma or by detecting low bone mineral density. There are different imaging modalities (Table) but dual energy X-ray absorptiometry is the preferred method.
Eligibility for treatment under the Pharmaceutical Benefits Scheme (PBS) requires confirmation of a minimal trauma fracture or low bone mineral density.
| Test | Radiation* | Sites | Advantages | Disadvantages | Clinical use |
|---|---|---|---|---|---|
| DXA | Minimal (4 microsievert) | Hip, spine, forearm | High precision, reproducible, correlates well with fracture risk | Affected by many artefacts, including previous fractures, spinal pathology, extrinsic artefacts, obesity | Hip bone mineral density best predictor for hip fracture. Lumbar spine bone mineral density best for monitoring treatment effect |
| QCT | High (200 microsievert at spine, 1200 microsievert at hip) | Hip, spine | Selective measurement of trabecular and cortical bone, true volumetric bone mineral density | Less reproducible, less standardisation, fewer analysis protocols | Sensitive for monitoring vertebral bone loss and treatment effect, especially in known spinal disease or artefacts |
| pQCT | Minimal (3–5 microsievert) | Distal bone (usually radius, tibia) | Compact and mobile machines | Small peripheral regions only, slow changes over time | Children |
| HR-pQCT | Minimal (5 microsievert) | Tibia, radius | Non-invasive measurement of microarchitecture, structure and mechanical strength | Small peripheral regions only, expensive machinery | Research tool for non-invasive determination of bone structure |
| QUS | None | Calcaneus, radius, tibia | Portable, no ionising radiation | Not standardised, operator dependent, poor reproducibility | May be able to predict fracture risk, but conflicting evidence for monitoring while on treatment |
* Daily background radiation approximately 5 microsievert, standard chest X-ray 20–60 microsievert.
DXA - dual energy X-ray absorptiometry
HR-pQCT - high-resolution peripheral quantitative CT
pQCT - peripheral quantitative CT
QCT - quantitative CT
QUS - ultrasonography
Vertebral fractures are often missed and can be asymptomatic, or present with progressive kyphosis, loss of height, or chronic back pain. A vertebral fracture can be defined as a 20% or greater reduction in anterior height versus posterior vertebral body height (see Fig.). The presence of a vertebral fracture is highly predictive of a subsequent fracture, but if the fracture is asymptomatic the patient may be left untreated and at risk.

In a large Australian community-based study of women aged over 70 and not known to have osteoporosis, thoracolumbar X-ray detected at least one vertebral fracture in 24.7%. In the same cohort, dual energy X-ray absorptiometry found 21.8% had osteoporosis at the femoral neck or lumbar spine. However, only 7.3% had both osteoporosis on dual energy X-ray absorptiometry and a vertebral fracture on thoracolumbar X-ray.2 Up to 50% of women with vertebral fractures have normal bone mineral density by dual energy X-ray absorptiometry, so potentially a third of women will not be diagnosed by this method.3
A thoracolumbar X-ray should therefore be performed in patients who have symptoms of a vertebral fracture, decreased bone mineral density on dual energy X-ray absorptiometry at the hip, or multiple clinical risk factors for osteoporosis. While spinal radiography is essential for diagnosing a vertebral fracture, it is important not to confuse the spinal deformity of an osteoporotic fracture from other causes including spondylosis.
Another method for detecting vertebral fractures is through vertebral fracture assessment using dual energy X-ray absorptiometry. Multiple studies have shown moderately good concordance between absorptiometry and thoracolumbar X-ray in identifying vertebral fractures.4-6 Limitations include adequate visualisation of the upper thoracic spine and potentially confounding spinal diseases.
By current criteria, a bone mineral density at the femoral neck equal to or less than 2.5 standard deviations below the mean for a young person of the same sex is diagnostic of osteoporosis. This is reported as a T-score of –2.5 or less. Prescribing criteria for antiresorptive treatment are based predominantly on the T-score, so measuring bone mineral density is usually required before treatment.
A screening measurement is reimbursed by Medicare for patients over 70 years old, in the absence of a minimal trauma fracture or secondary cause of osteoporosis. For patients who have sustained a minimal trauma fracture, measuring bone mineral density is not required for the diagnosis of osteoporosis or to fulfil some PBS prescribing criteria for osteoporosis. However, a baseline measurement is useful before starting treatment.
The Z-score is the number of standard deviations away from the mean bone mineral density of a person of the same age and sex. A Z-score below –2.5 should raise suspicion of a secondary cause of osteoporosis.
The most commonly used technique for measuring bone mineral density is dual energy X-ray absorptiometry. This harnesses the high sensitivity of calcium in absorbing X-rays to measure the relative amounts of bone and other soft tissue, in order to calculate bone mineral content and hence density (Table). Absolute measurements from different machines differ significantly so standardised reference ranges should be used. Serial measurements should be performed on the same machine to identify true changes in the patient’s bone mineral density.
Dual energy X-ray absorptiometry is versatile and can be used to measure bone mineral density at various body sites. Of the four potential sites at the hip (total hip, femoral neck, trochanteric region and Ward’s triangle), the density of the total hip is recommended due to its high precision, reproducibility and correlation with fracture risk.7 Measurements at the lumbar spine are also highly reproducible, but can be heavily influenced by artefacts. The forearm may be used when the hip or spine cannot be measured or interpreted, but there can be a significant difference in bone mineral density between the dominant and non-dominant arm.8 Current evidence shows that bone mineral density at the hip is the most reliable for predicting hip fracture risk, and spinal bone mineral density should be used for monitoring treatment.9
Technical factors can affect measurements made by dual energy X-ray absorptiometry. Commonly there are false elevations due to vertebral disease, such as osteoarthritic spondylosis, osteophytes, scoliosis or vertebral fracture, or extrinsic artefacts from calcifications and surgical metalwork. Obesity may alter the calculated bone mineral density. Osteomalacia may lead to underestimates due to decreased bone mineralisation. Acquisition errors in patient positioning and other physical artefacts can usually be overcome by trained staff, quality control and regular services of the machines. Correct positioning is critical for accurate measurements and should be confirmed by the clinician. For optimal hip measurements, the femur should be internally rotated so that the lesser trochanter is not seen. Spine images should be centred, straight and not rotated.
Quantitative CT generates a reconstructed three-dimensional image and calculates bone density when calibrated to a reference object of known density. It measures true volumetric bone mineral density and is not limited by the patient’s size or vertebral deformities.10 Results can occasionally be spuriously low in a patient with normal T-scores on dual energy X-ray absorptiometry. It is suspected this is due to increased marrow fat with advancing age which affects the assessment of bone density when measured by CT. Quantitative CT may also be used to assess a patient who is suspected of having a falsely elevated bone mineral density on dual energy X-ray absorptiometry due to osteoarthritis. Limitations of CT include higher doses of radiation, less reproducibility and fewer standardised reference ranges and analysis protocols.
Peripheral quantitative CT requires machines specifically designed for distal bone sites (usually radius or tibia). Its use is mostly limited to children.
High-resolution CT has spatial resolution that allows imaging of individual trabeculae. This is a non-invasive method of viewing three-dimensional microarchitecture and trabecular and cortical structure. Radiation is minimal, scan time is relatively short (approximately three minutes) and scan precision is acceptable, making this an attractive method for determining bone structure, although it is currently limited to research centres.
Ultrasonography calculates bone stiffness as a surrogate for bone density and is most commonly used on the calcaneus.11 Clinical studies suggest that ultrasonography can predict hip fractures12 and vertebral fractures13 in a similar way to bone mineral density. Benefits include no ionising radiation, and portability of the machine. Its limitations include significant manufacturer and operator differences. Ultrasound is not currently recommended for screening for osteoporosis.
Apart from low bone mineral density, a number of clinical risk factors for fractures have been identified and should be used together with the bone mineral density to calculate an individual’s fracture risk (Box 1).14,15 Peak bone mass is achieved by age 30. Bone loss occurs steadily from the age of about 40 (0.3–0.5% per year), with accelerated loss in the perimenopausal period (4–6% per year) before slowing again after the age of 70 (1–2% per year).16 Age is therefore the strongest predictor for fracture risk.
Box 1 Clinical risk factors for fracture 14,15
Age >70 years
Low body weight or significant weight loss
Physical inactivity (including secondary to chronic illness or spinal cord injury)
Drugs: corticosteroids (≥5 mg prednisolone daily or equivalent for ≥3 months), anticonvulsants, thiazolidinediones, selective serotonin reuptake inhibitors, thyroxine, aromatase inhibitors, chemotherapy
Current smoking
Alcohol (≥2 standard drinks/day)
History of fragility fracture
Parental history of hip fracture
Low sunlight exposure
Although bone mineral density provides an estimation of osteoporosis, it is insufficient for predicting an individual’s fracture risk. Clinical risk models, such as the FRAX tool17 and the Garvan fracture risk calculator18 use bone mineral density and clinical factors to predict an individual’s absolute fracture risk. The patient’s risk of falls is also essential in risk stratification.
FRAX* has been the most extensively used tool worldwide and calculates the 10-year risk for a hip or major osteoporotic fracture (hip, clinical spine, humerus or wrist). By combining clinical risk factors with bone mineral density and age, the sensitivity of fracture prediction improves without reducing specificity. A 10-year probability of a hip fracture more than 5%, or of a major osteoporotic fracture more than 20%, is significant and antiresorptive treatment should be considered (see case study in Box 2). The main limitation of FRAX is the dichotomised risk factors (presence or absence of a parameter) rather than quantifying each risk factor. For example, two previous fractures increase the risk much more than a single previous fracture, and increased total consumption (duration and dose) of glucocorticoids, tobacco and alcohol are associated with greater fracture risk. A further limitation is that the algorithm only uses the T-score measured by femoral neck dual energy X-ray absorptiometry. The applicability of FRAX to patients with discordant T-scores at other sites or the use of different technologies has yet to be determined.
The Garvan fracture risk calculator can be used with or without a measurement of bone mineral density. It quantifies the number of fractures and takes into account the patient’s history of falls. The calculator gives both a 5-year and 10-year risk for a hip or any fracture and is useful when a measurement of bone mineral density cannot be performed or interpreted. Its main limitation is the absence of other clinical risk factors in the risk calculation.
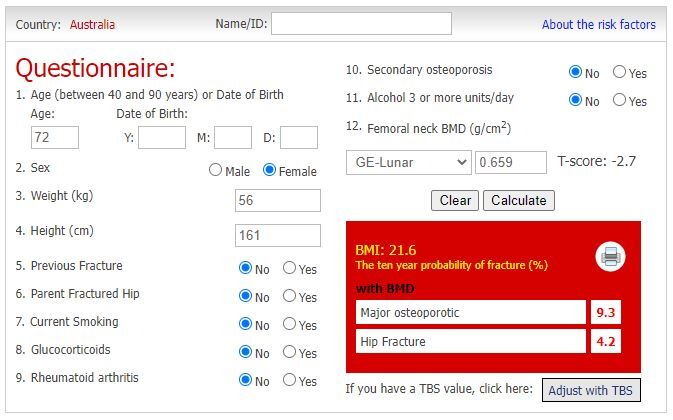
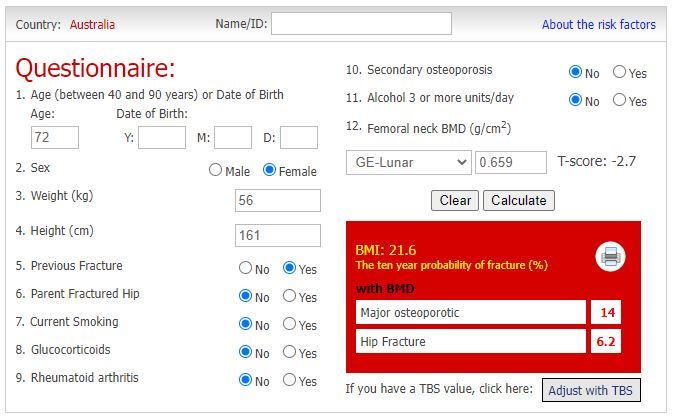
Box 2 Case study: calculating fracture probability17
A 72-year-old female with no personal or family history of a fracture and no other high-risk features and a femoral neck bone mineral density T-score of –2.7, has a 9.3% probability of any osteoporotic fracture and 4.2% probability of a hip fracture in 10 years (see A). If the same patient had previously sustained a fracture, her probabilities would increase to 14% and 6.2% (see B), placing her at high risk of hip fracture and therefore treatment would be warranted.
Osteoporosis is a common disorder that affects many Australians. Preventing fractures is crucial to reducing the associated morbidity and healthcare costs.
Diagnosing osteoporosis requires a careful search for fragility fractures and measuring bone mineral density. Thoracolumbar X-ray may reveal an asymptomatic vertebral fracture, which significantly increases the individual’s risk for a further fracture. Dual energy X-ray absorptiometry is the preferred method of measuring bone mineral density as it has excellent precision, minimal radiation and is useful in predicting a fracture and for monitoring treatment. Combining the bone mineral density with clinical risk factors in risk calculators can quantify a patient’s fracture risk and can guide specific treatment.
Advanced trainee, Department of Endocrinology, St George Hospital
Conjoint associate lecturer, University of New South Wales, Sydney
Senior endocrinologist, Department of Endocrinology, St George Hospital
Associate professor, Endocrinology, University of New South Wales, Sydney